Guest Article By Dr. Alan Christianson
Guest Article By Dr. Alan Christianson
This is a guest article, written by Dr. Alan Christianson. Dr. Christianson is a NY Times Bestselling Author and Naturopathic Medical Doctor who specializes in natural endocrinology, especially thyroid and adrenal disorders.
Saturated Fat – Is It A Magical Elixir For Your Brain?
 It seems that everywhere I look there is another article claiming that saturated fat as found in butter, animal fat, or coconut oil, is a magic elixir for your brain.
It seems that everywhere I look there is another article claiming that saturated fat as found in butter, animal fat, or coconut oil, is a magic elixir for your brain.
I would like to address a few representative quotes I found recently and then go through the current research on saturated fats and brain function. I think you will be shocked.
In an article called “How Eating Fat Can Make You Smarter,” I read that: “Saturated fat is actually one of the main components of brain cells, and is, therefore, necessary for healthy brain function. In one study, it was found that people who ate more saturated fat reduced their risk of developing dementia by 36 percent.” [1]
I read the study that was cited. Oddly they never used the number ‘36’ anywhere. In fact, the only time the word saturated was used was here:
“ The . . . NIH . . . recently commissioned an independent . . . report that included a comprehensive systematic review of the evidence related to risk factors for AD and cognitive decline. . . . The factors with the most consistent evidence included diabetes mellitus, current smoking, depression, cognitive inactivity, physical inactivity, and poor diet (high saturated fat/low vegetable intake)” [2]
Not only did they not say saturated fat cut your risk of developing dementia by 36% but they actually said that saturated fat intake was one of the most documented risk factors for causing dementia.
Another paper argues that your brain needs saturated fat to keep your brain cells insulated.
“Your brain is about 60% fat, 25% of which is cholesterol. If you’ve ever tried a low-fat diet and felt tired or unfocused all the time, you now know why: you’re starving your brain of one of its main components. No surprise that low cholesterol links to cognitive decline.” [3]
Here is a quote from the actual study that the above paper referred to: “Brain cholesterol is synthesized in situ by astrocytes and oligodendrocytes and is almost completely isolated from other pools of cholesterol in the body . . . The major apolipoprotein constituent of HDL in the CNS is apolipoprotein E, which is produced by astrocytes and microglia. Apolipoprotein A-I, the major protein component of plasma HDL, is not synthesized in the CNS” [4]
What does this mean? It means that your brain does need cholesterol and saturated fat, but it makes its own when it needs it.
Roughly 7% of your circulating cholesterol comes from your diet. Your brain is not dependent on your diet for cholesterol. Your brain makes its own cholesterol as needed and that cholesterol is made from different constituents than the cholesterol in your bloodstream.
Your brain does not run out of cholesterol or saturated fat the minute you stop drinking coffee with butter in it.
Another author cited a study and said that it proved saturated fat helped the brain. He said “individuals eating more of the “dreaded” fat actually have a substantial risk reduction.” [5]
Yet the researchers themselves did not say that saturated fat caused a reduction of risk. In fact, they said there was no trend suggesting that saturated fat reduced risk. Regarding saturated fat and dementia, “the tests for trend were not significant.” [6]
I have even read endorsements that said: “I Believe Over Half of Your Diet Should Be Made Up of Saturated Fat” [7]
What science tells us about saturated fat.
OK, What does science tell us?
The most comprehensive clinical review to date that specifically looked at types of dietary fat and rates of dementia found that: “Several lines of evidence provide support for the hypothesis that high saturated or trans fatty acids increase the risk of dementia. Of all the different types of fatty acids, the findings are most consistent for an increased risk of cognitive decline with a higher intake of saturated fatty acids.” [8]
Four large studies looked at the relationship between saturated fat and Alzheimer’s disease. Another four looked at how it may affect mild cognitive impairment (MCI) and four looked at its effects on cognitive decline. [9]
None of these studies suggest any protective role for saturated fats and brain function.
In fact, the vast majority of these studies showed that saturated fats worsen Alzheimer’s disease, MCI, and cognitive impairment.
The largest study on saturated fats and total longevity showed that: “When compared with carbohydrates, every 5% increase of total calories from saturated fat was associated with an 8% higher risk of overall mortality” from causes like Alzheimer’s disease, cardiovascular disease, and cancer. [10]
Many parts of your body do use saturated fat and cholesterol. However, these are not essential fats. In the body’s natural state it can make as much of these fats as it needs, whenever it needs them.
That does not mean that they are harmless. A common thread among all societies found to have higher rates of longevity and lower rates of chronic disease is that they have diets low it total fat and low in saturated fat.
Saturated fats are not a health food and there is no credible evidence suggesting that they will protect your brain from aging or help it work better.
I felt compelled to directly counter these points because the vast majority of available evidence says the exact opposite. The more of it you consume, the greater your risk is for early death and brain impairment.
 This was a guest article written by Dr. Alan Christianson.
This was a guest article written by Dr. Alan Christianson.
Dr. Christianson is a NY Times Bestselling Author
and Naturopathic Medical Doctor
who specializes in natural endocrinology,
especially thyroid and adrenal disorders.
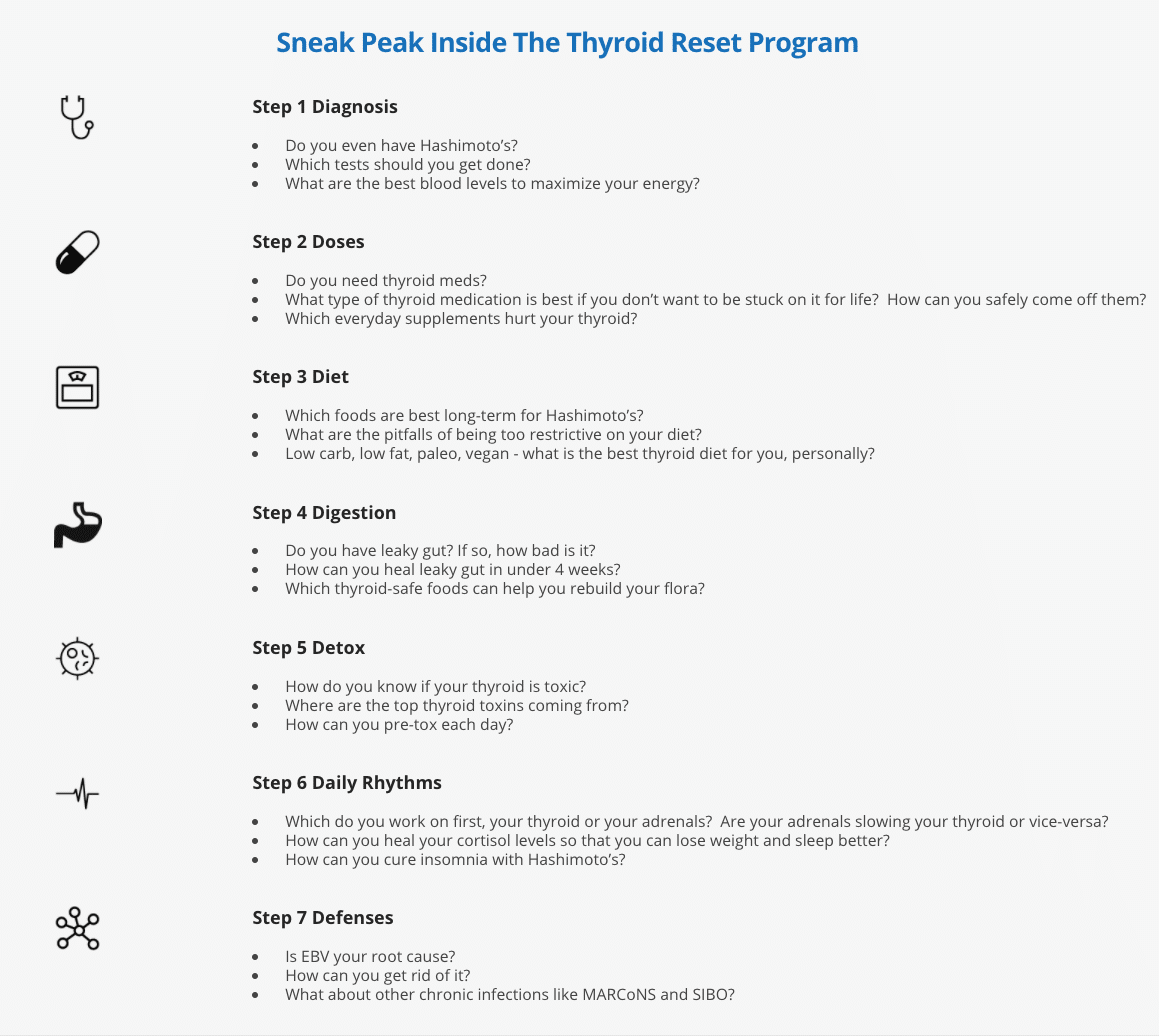
Dr. Cs’ new Thyroid Reset Program
Note from Ari: For any of you with hypothyroidism, I want to mention that Dr. Chrisitianson just released his completely revamped Thyroid Reset Program. He did just re-did the entire program and it’s packed with the latest and greatest science on optimizing your thyroid health and reversing the symptoms of hypothyroidism. What exactly does your thyroid affect? Weight. Hair. Energy. Healing. Autoimmune. Dementia. Heart health…. The list is long. LIFE long. If you have hypothyroidism, this is a must-have program. (Dr. C has also made it incredibly low-cost, so it’s affordable by everyone). You can grab it here.
(Note: Registration for the program closes tonight at midnight, May 1st, so today is the last day to get in. Click here if you want to learn more about it)
Case studies
Below are a few case studies Dr. Christianson wanted to share about people who have gone through his Thyroid Reset Program.
Case study 1
‘Anne’ signed up for the program hoping to lose 25 pounds and stop her progressive hair loss. No matter how strictly she dieted, her weight did not budge. Her hair loss kept going even though she hoped her biotin would help. Her current diet was strict autoimmune paleo with no nightshades, legumes, or dietary goitrogens.
At age 53, Anne started thyroid treatment about five years ago. When she started the program she was taking:
- Levothyroxine 100 mcg
- Thyroid support supplement with 200 mcg iodine
- Biotin 5000 mcg
Her blood tests were last done just a few weeks before starting the program. She had no changes to her treatments or diet since then.
- TSH 3.8 U/mL (optimal range 0.4 – 1.5)
- fT3 1.7 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.8 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin 1400 IU/mL (optimal range <1)
- Anti thyroperoxidase 120 IU/mL) (optimal range <1)
- Ferritin 14 ng/mL (optimal range 70 – 180)
From the things she learned in the program she made a couple of changes:
- Switched to Natural thyroid at a lower dose
- Found out she was anemic and started treating it more effectively
- Stopped taking iodine supplements
- Stopped taking biotin in high doses since it can skew her thyroid tests
- Added back legumes and potatoes to her diet
Anne wrote in to share her excitement about the changes she saw before the end of the 7 weeks:
- “My weight just dropped 10 pounds right after changing my meds!! And I was taking less!!” It has gone down a total of 8 pounds more for a total of 18 pounds.
- Her hair loss also stopped and she’s seeing some early signs of new growth.
Her results also showed major changes:
- TSH 1.8 U/mL (optimal range 0.4 – 1.5)
- fT3 3.7 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.6 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin 235 IU/mL (optimal range <1)
- Anti thyroperoxidase <1 IU/mL) (optimal range <1)
- Ferritin 93 ng/mL (optimal range 70 – 180)
Moving forward Anne is optimistic she will see further weight loss, hair growth, and reduction in her thyroid dosage.
Case study 2
‘Nicole’ signed up for the program mostly because she was not sure if she was on the best thyroid treatment. She was on a new regime as of the last few months and had been getting palpitations, insomnia, and hair loss. She saw a new doctor hoping to lose weight and he put her on a T3 only medication.
She had been doing a low carb diet but had occasional gluten and dairy.
When she started the program she was taking:
- Cytomel 50 mcg
- A multivitamin with folic acid and iodine
- Prilosec OTC for heartburn
- Bone broth protein
Her blood tests were last done just before starting the program. Her prior doctor did not believe in testing her levels but she insisted. He would not test her antibody levels.
- TSH < 0.001 U/mL (optimal range 0.4 – 1.5)
- fT3 8.6 pg/mL (optimal range 2.3 – 4.5)
- fT4 0.7 ng/dL (optimal range 1.09 – 1.9)
From the things she learned in the program she made a couple of changes:
- Found a new physician to work with
- Switched to Natural thyroid at a much lower dose
- Stopped supplements with folic acid due to the cancer risk
- Saw a cardiologist and found her last medication put her in atrial fibrillation
- Changed to a thyroid-specific multivitamin
Over the course of the 7 weeks, Nicole learned that the palpitations, insomnia, and hair loss were all likely side effects of a thyroid dose that was far too high. These symptoms resolved but she’s not yet seen hair regrowth.
Her post program results were much better:
- TSH 0.8 U/mL (optimal range 0.4 – 1.5)
- fT3 3.1 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.3 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin <1 IU/mL (optimal range <1)
- Anti thyroperoxidase <1 IU/mL) (optimal range <1)
Nicole needed to drop her thyroid dose several times during the 7 weeks. She was surprised when she learned in the program that an overdose of thyroid could cause someone to hold onto extra weight. She did notice her clothes fitting looser as her scores got better.
Her new doctor performed her first ultrasound and saw no signs of Hashimoto’s or other problems with her thyroid. She and her doctor are optimistic and think she may soon not need long-term thyroid treatment.
Case study 3
‘Jackie’ joined the thyroid program because of her severe fatigue and muscle pain. She’d been diagnosed with both fibromyalgia and chronic fatigue over past few years and was on medical disability because the fatigue was so severe. She rated her energy levels between 1-2 out of a possible 10 on most days and 3-4 out of 10 on her best days which happened just a few times per month.
When she started the program she was taking:
- Synthroid 150 mcg
- A multivitamin with folic acid and iodine
- Adderall for focus and energy
- Ambien for sleep
- Soma for muscle pain
Jackie’s last blood tests were last done nearly a year before starting the program. She did not have follow up labs to share.
- TSH 4.1 U/mL (optimal range 0.4 – 1.5)
- fT3 1.6 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.5 ng/dL (optimal range 1.09 – 1.9)
After starting the program she did additional testing and learned some new things.
- She had celiac disease and was not absorbing her medication properly
- She had no thyroid antibodies and a clear ultrasound
- She was positive for chronic Epstein Barr Virus.
Over the course of the 7 weeks of the program, Jackie changed to natural thyroid, did treatment for EBV, and went strictly gluten-free, and started carb-cycling. Jackie was also able to stop her Adderall, Soma, and Ambien.
Some combination of these changes pulled her out of chronic fatigue. First, she was able to regain her natural sleep and get her energy back. She ended the program with energy levels of 6-8 most days.