Dr. Alan Christianson is a NY Times Bestselling Author and Naturopathic Medical Doctor who specializes in natural endocrinology, especially thyroid and adrenal disorders. He’s also a good personal friend of mine who I’ve had the privilege of getting to know and geek out on science with, and I can tell you without any hesitation that he’s one of the most brilliant and knowledgeable people in the entire health industry.
Did you have hypothyroidism? Or do you suspect you might? Then this interview is must-watch material! In this interview, you’ll learn:
- How to know if your thyroid is causing your symptoms
- Why the majority of people with hypothyroidism are getting misdiagnosed and mistreated
- The best thyroid medication to be on
- Why iodine — which is commonly found in thyroid boosters and many supplements — can actually WORSEN your hypothyroidism
- Whether grains and gluten are the cause of autoimmune conditions and hypothyroidism
- Dr. Cs’s CRAZY results from sending out patients’ blood for food intolerance testing
- Why healing your gut is so important to fix your thyroid (and the most powerful foods for healing the gut)
Dr. Christianson has also just released an amazing new program on reversing hypothyroidism called the Thyroid Reset program. It’s packed with phenomenal content (he just redid his entire course over the last couple months). If you have hypothyroidism, this is a must-do program. You can get The Thyroid Reset program here. (Be aware that registration closes in just a few days, on May 1st.)
Download or listen on iTunes
Listen outside of iTunes
Watch
7 Steps To The Ultimate Thyroid Fix – Transcript
Ari Whitten: Everyone, I’m here with Doctor Dr. Alan Christianson, and it is my absolute privilege and honor to introduce you to him.
I met Alan in person about a year ago, and we kind of just hit it off. He’s become my man crush, my bromance because he and I are very, very like-minded in a lot of sense, and he’s really just a thought leader in this field. In the true sense of that word, I happen to know a lot of people in this industry, and everyone really looks up to Alan with a lot of admiration, and they look to him as a source of knowledge and expertise on this subject.
The reason why is Alan is really, really, truly an expert in the true sense of that word. He really goes to the science, and most importantly and what I really love about him the most is his allegiance really lies with the science itself.
A lot of people out there are drifting along with whatever the popular fads are of the day, and Alan doesn’t do that. He stays true to whatever the science says and whatever the science says is what you’re going to hear from him. That is why he is really regarded as one of the world’s foremost experts in this whole area of thyroid conditions, adrenal conditions, fatigue, and energy enhancement. With all of that said, I still feel like I’m not doing you justice, but with all that said, let me introduce you to Dr. Alan Christianson, so how are you today?
Dr. Alan Christianson: I’m doing awesome. Always glad to be with you Ari, and that was a beautiful, beautiful intro. Greatly appreciated.
Ari Whitten: You’re welcome.
How to know if you have a thyroid condition
With that said, let’s get right into it. Tell me a little bit about thyroid stuff. Let’s talk thyroid conditions. First of all, some of the symptoms that go along with thyroid conditions can be kind of vague, and they can … Maybe certain people might have fatigue, they might have weight gain, or hair loss, or things like that, and how does one know when they have a thyroid condition or how do you know when someone has a thyroid condition?
Dr. Alan Christianson: Awesome question and the symptoms are really nebulous. If you look at some lists that are put out about all the possible thyroid symptoms, everyone every day at any moment would be suspecting it, because any symptom can be relevant.
Back in ’95, there was a study called the thyroid … Colorado thyroid prevalence study and they had a public health fair. They had about 20,000 people come through this, and they gave them pretty detailed symptom questionnaires, and they also gave them thyroid blood tests.
In a perfect world they would have used more stringent parameters for how they looked at the results, but nonetheless, they partitioned people into having normal thyroid status, overactive, and underactive.
Then the exciting part was, they looked back afterward and looked at the surveys of those corresponding people, and they saw which symptoms were the most predictive both in terms of positive predictive value and also negative predictive value. Which symptoms pointed towards having a thyroid problem, and which symptoms in their absence pointed away from that problem.
From that there were some really nuanced things I learned about symptoms, so one of which was that there are about 11 big symptoms that are somewhat predictive, and I probably won’t get them all right, but it’s really all around hoarseness was a big part, changes of hoarseness, swallowing, speech, yes, fatigue was a factor, weight changes, hair changes, also cold intolerance, some of the muscle pain, which showed up quite a bit. Many of these symptoms were put both in terms of, for example, hoarseness but also more hoarseness, so there was a sense of a static symptom, but also of a more dynamic nature.
Some nuanced things I got from that, one of which was that people with thyroid issues, there’s really no good exclusionary symptoms. There are no symptoms that had a strong negative predictive value, none that were above 30%.
I’ve seen many people look at a list of thyroid symptoms and say, “Well, but I’m not gaining weight. That can’t be me.” No, it still could be, because many are not having that particular symptom. I almost imagine there’s this deck of, say, a dozen cards, and the deck gets shuffled and someone gets passed out typically two to four cards, so that was the real mean number of symptoms was two to four was most typical.
It was not common to have many more and it was not common to have many fewer. You get a couple of symptoms, and they’re a completely different set of symptoms from person to person.
Then the other big thing was that the change dynamic symptoms had more of a positive predictive value.
When someone says, “Hey, I’ve had … I’ve really been crashed in my energy. I’m gaining weight for no clear reason.” Then the next question is, “Well, how long has it been going on?” “I guess I always struggle with that.” Little less suspicious. That same person, “Oh, yeah, like last January went to hell in a hand basket. It all switched right around then.” That’s really suspicious. When there’s a definite timeframe, there’s a clear progression or shift in symptoms, that’s more likely as well.
Ari Whitten: Interesting. Yes, please.
How 40% of people with Hashimoto’s are at risk of misdiagnosis
Dr. Alan Christianson: Someone suspects Hashimoto’s and they get a diagnosis.
What happens in a parallel scenario very commonly is someone suspects Hashimoto’s and they’re told they do not have it. They go to a doctor and the scenario is that they think they’ve got a thyroid problem, and maybe their levels of thyroid function are reasonable, perhaps not great, but they’re reasonable, and there are no blood markers of Hashimoto’s. There are no measurable thyroid antibodies, so there are thyroid peroxidase and thyroid globulin antibodies that are measured for.
Almost all doctors don’t understand that these antibodies do not have a strong negative predictive value. They’ve got a perfect positive predictive value, so if you’ve got the antibodies there, you’ve got Hashimoto’s, but the absence of the antibodies is not the absence of Hashimoto’s.
More than 40% of people with Hashimoto’s never have measurable antibodies. That’s just one thing I wanted to throw out there in that diagnosis part, because so often someone is turned away and said, “Oh, it’s something else because you’ve got … you’re negative for Hashimoto’s.”
Ari Whitten: Yeah, and that’s interesting because there’s this category of hypothyroidism that … I know that there’s such a thing as non-Hashimoto’s hypothyroidism, but from my understanding, it seems like a lot of people who are being told they have hypothyroidism but don’t have Hashimoto’s actually do have Hashimoto’s.
What the different categories of diagnosis are
Dr. Alan Christianson: Yeah. In almost all cases it’s just not a thorough diagnosis. Hashimoto’s, you know in medicine we’ve got different categories of diagnosis.
We’ve got syndromes, which are probably the worst. That’s like a constellation of symptoms that cluster together, and then we have diagnosis of empirical finding. You break your leg and here’s the picture on the X-ray. Then other diagnosis are actually histologic diagnosis.
To be really precise Hashimoto’s is a tissue analysis, a histologic diagnosis, so the only rule out is to remove someone’s thyroid and do a thorough analysis of multiple points of that under a microscope. That’s the only definitive rule out.
Why a biopsy will not rule out Hashimoto’s
Ari Whitten: To remove the whole thyroid or to do a biopsy.
Dr. Alan Christianson: A biopsy is not a definitive rule out, because a biopsy … With a biopsy, you’re looking at basically 10 square meters of America from a satellite, and you could say America is one big parking lot. Parts of it are, but not all of it.
Ari Whitten: Yeah. Good point.
Dr. Alan Christianson: Biopsies have positive meaningful value, but they don’t have strong negative meaningful value. You can’t rule things out. It’s only by full analysis.
How Hashimoto’s is a presumed clinical diagnosis
Ari Whitten: That full analysis of the histological examination sounds like a test that I hope I never get.
Dr. Alan Christianson: It’s not a test that we ever do. You’re right. It’s really a presumed clinical diagnosis, and someone who’s hypothyroid in the absence of another explanation, we assume that’s Hashimoto’s.
There are some scenarios of other explanations, so someone that had a thyroidectomy for cancer removal, in many cases they also had Hashimoto’s, but nonetheless, that could be a reason for it, or there are those who are on lithium, mostly for bipolar disorder, that can suppress the thyroid. There’s those who have had past treatment for hyperthyroidism and they’ve had their thyroid radioactively ablated or there are those who had radiation treatments to the neck, more so historical – it’s crazy, but that was a common thing for sore throats back in the 50s. You’d get your neck irradiated. – Some of those people became hypothyroid. Apart from, honestly, not much more than those few criteria, it’s Hashimoto’s.
What the optimal reference range on thyroid hormone tests is
Ari Whitten: Let’s talk about reference ranges now, because part of the testing for thyroid conditions is this very black and white sort of … In terms of the way that most physicians would analyze the numbers on the thyroid hormone test, it is very black and white in how they interpret it.
It’s like are you within the reference range either at the very bottom, or the middle, or the very top, and then regardless of where you are, you’re told nothing is wrong. Then as soon as you go just a tiny bit outside of that below the reference range, all of a sudden something’s wrong. Can you talk a little bit about what’s normal versus what’s optimal as far as those reference ranges?
Dr. Alan Christianson: For sure. This is an area to where, I don’t know, it’s a big illustration of … I was a stalker of you before we first met, so you have the same thing. I really respect you about following the truth, looking at the research, not getting caught up in fads. The downside about…
Ari Whitten: That’s why I said it’s a bromance, and now I’m fortunate that we’re actually friends and I can talk to you on the phone and bounce ideas off you and things like that, and get your opinion and your insights.
Dr. Alan Christianson: The only bad thing about being so fervent to sticking away from fads is that a lot of times it’s just you and me and the truth all by ourselves. There’s not always a lot of company.
Ari Whitten: I know exactly what you mean.
Dr. Alan Christianson: Here’s a case where I part company with the conventional and the alternative sides. The conventional side you illustrate it pretty well. There are a few tests. There’s a big barn door you’ve got to hit. If you hit the barn door, they call it good.
The alternative side says you can ignore the tests because they’re all junk, and neither of those is really that great. The tests we think about as tests of the body asking the thyroid to work, and that’s TSH, thyroid stimulating hormone, and there’s the test of the thyroid hormone output, which is T3 and T4.
When you take people and you pull out everyone that has any inkling of thyroid problems and you give them these same tests over and over again, an interesting thing emerges. The free T3, free T4, the thyroid output is actually about the same in that group as it is in the reference range.
The alternative world says you’ve got to be high T3, high T4. Healthy people aren’t. Healthy people have a big distribution of those hormones. The TSH is different. The TSH is a backwards marker, so since it’s your pituitary telling your thyroid to work, when the gland is underactive it gets yelled at, and the TSH goes higher.
If it’s overactive your pituitary is like, “Whoa, I’m not going to ask you to do anything. You’re out of control,” and it goes lower. It’s inversely related.
Healthy people have in the normal range but on the bottom end of the normal range compared to normal levels, so in terms of absolute numbers most labs say that .4 to 4.5 or 5.5, that’s what they call the normal range, but healthy people, they don’t run lower than .4, but they also don’t run higher than about 1.9 ever.
Most scores are really close to about .99 in healthy people. They’re that bottom end of the normal range for the TSH.
Ari Whitten: What’s the high end of the range? Doesn’t it go up to 7.5 on a lot of tests?
Dr. Alan Christianson: It does vary from lab to lab. You’re right. In my region, I see 4.5 most commonly. Many say 5.5. Some say higher than that.
When I started practicing, 12 was standard. You could be up to 12 and most would say, “Oh, you’re something else. You’re fine. You’re just bellyaching about this.”
Ari Whitten: That’s quite a range, huh, from .4 to 7 or 12.
Dr. Alan Christianson: Yeah.
The standardized thyroid hormone medication
Ari Whitten: What about medications, so I know that there are the standard recommendations around usually just T4 is given, and then there are other opinions more on the alternative or functional medicine community. They talk about mixes of T4 and T3 or compounded T3, and natural desiccated thyroid. What’s the deal on all that? Where do you want to start looking at things other than the standard T4?
Dr. Alan Christianson: T4 only is, you’re right, it’s real standard of care. And, I’m not a conspiracy guy, but there’s a lot of collusion between Abbott Laboratories and the educational world in the conventional side.
The American Academy of Clinical Endocrinology is highly funded by them, and Synthroid’s…
Ari Whitten: Is Abbott Laboratories the ones who make T4?
Dr. Alan Christianson: They make Synthroid, which is the most popular brand name product of T4. There are generics also.
Back in the 80s, we didn’t have the current level of standardizing for thyroid medications so thyroid medicines all have iodine, and the synthetic medicines, the iodine is solely within the active hormone.
Natural desiccated thyroid is ground up pig thyroid, and it also contains iodine but not exclusively within the hormone content. So, if you’ve got a T4-only medicine, you can assay for iodine and you can be pretty confident that that will reflect the hormone activity.
In a natural product, if you only assay for iodine, you won’t get as perfect of a reflection of the hormone activity, because there’s a lot of iodine that’s not hormonally bound.
That was the disconnect back during the Carter administration. There were many brands of natural thyroid that met standardization guidelines but were not consistent in their potency, and that was a real problem. The earlier marketers of Synthroid pointed that out, and they gave a case study in a JAMA article in ’79. It was a sad story.
It was a woman who was obviously undermedicated even though she should have been on a potent enough medication, but the problem was the manufacturer.
Before then, most doctors did prescribe natural thyroid, but in the ensuing years it completely flipped, and now it’s just standard of care to use synthetic.
The wrinkle is that that issue of standardization, that changed in ’82. Now the standardization in terms of the tablets is not based upon iodine content but on active hormones. When they say that the natural thyroid is not standardized as well, that was true during the Carter administration, but it’s not true today.
Ari Whitten: Interesting.
Dr. Alan Christianson: The synthetic is primarily T4 or T3, and you mentioned there’s compounded combos of those. The natural has T4, T3, but also T2. And T2 seems to be an unsung hero in terms of affecting metabolic rate and energy production.
Ari Whitten: Yeah. I’ve seen some supplements that are more targeted towards people in the fitness industry that actually have isolated T2 in them.
I’ve seen some interesting research on that being an effective fat burner. It’s not very conclusive data by any means, but there’s some interesting preliminary data on benefits of T2. Natural desiccated thyroid may have some stuff that the medications don’t have.
Dr. Alan Christianson: That’s correct, and there’s some rather dated but still useful information showing how people who have had a thyroidectomy if they’re on T4-only, their T2 levels are non-measurable, whereas someone who has their own thyroid output, they’ve got a certain range of T2.
Yes, there is data like you were saying, saying how it does affect energy output, metabolism. The other funny thing is that T2 does not affect TSH, so whether you’ve got it or not, you wouldn’t really know that based upon your scores. You can look like you’re fine even though you’re really missing out on something important.
Dr. Christianson’s preferred thyroid medication
Ari Whitten: Interesting. As far as your recommendations for the people that you work with in your clinic who have hypothyroidism, what do you typically recommend? Do you go more the desiccated thyroid route, or more of the standard of care, or more T4, T3 combinations? What’s your general take on, like, is there a universal recommendation or is it a case by case thing?
Dr. Alan Christianson: The criteria I think about, the ideal medication would have all the active hormones, the three hormones that I mentioned. The ideal one would be well standardized, very consistently manufactured, and there are some brand variances in all versions of that.
The ideal one would also be free of binders or fillers. Thyroid medications are very different from vitamin C or calcium or magnesium because this is all stuff in the microgram world.
A milligram is about the mass of a grain of salt, and a microgram is like seven-thousandths of that, which we can’t really fathom or visualize. At that size of scale the whole physics of binders, or fillers, or uptakes become very, very significant, and can have a big effect upon how that medication works.
Given all those criteria, my preferred medication is WP Thyroid, which is an exact product name, and that’s one that has the best standardization. It’s better standardized than the synthetics are. It’s natural thyroid. It’s also free of binders or fillers, so that’s my real go-to.
Compounded medications, I love the concept. A couple of drawbacks, they do not contain T2. There are also thyroid proteins found in desiccated thyroid which can lower the autoimmunity, so the compounded ones do lack that. The biggest thing about the compounding is that there’s no standardization post-production. They’re made and there are no real legal requirements to have them assayed.
Ari Whitten: Interesting. Now the problem of standardization is on the isolated T4 and T3 rather than the desiccated thyroid.
Dr. Alan Christianson: These things in a compounded form, again, they’re micrograms, so there’s a case that I will never forget about, a patient of mine was prescribed by another doctor a compounded thyroid, and it was meant to have had 7.5 micrograms of T3, which is not unreasonable, but it actually contained 7.5 milligrams of T3.
You and I know that’s a big deal, but it sounds like a small thing. This person spent about three months connected to life support, and she survived in a vegetative state just barely.
That’s how powerful thyroid hormones are, and that’s why I just don’t even have any comfort with things I question. If I’ve got to know that it’s dependent upon the skill of one person or one company: no. I’m just not good at that. I just want to know it’s going to be okay.4
How conventional practitioners ignore diet as part of Hashimoto’s treatment
Ari Whitten: I hear you. Yeah. For sure. Let’s talk a little about diet, so nutrition as it relates to autoimmune conditions in general, but also Hashimoto’s specifically.
I know that there are some controversies in here. You have a lot of people out there in functional me- … I guess we’ll start with the conventional medical community, where they’re basically ignoring [inaudible].
Dr. Alan Christianson: That’s a pretty simple discussion.
Ari Whitten: Yeah. End of discussion. There’s nothing to discuss. I mean that they basically ignore nutrition altogether, and the idea that there are certain things that can be done with nutrition that can affect thyroid function, I think, for most conventional medical doctors is kind of laughable. They don’t even really pay any attention to it because they think, as far as I can see, they think it’s insignificant and that it doesn’t really have any effect. Do you have any thoughts just on the power of nutrition in general? Can you actually influence thyroid health through what you’re eating?
The inconsistency of thyroid antibodies
Dr. Alan Christianson: You can, positively and negatively. Just one thing to really preface this discussion would be the sense that there’s a natural progression of Hashimoto’s, and probably 20, 25% of it will have it go into remission. That may or may not be dependent upon their actions.
Maybe they wore blue socks on Tuesday and their Hashimoto’s went away, and that’s … It may not have been the blue socks that helped. There are some to where it does just go away on its own accord. Then even along those same lines, thyroid antibodies are extremely nebulous lab markers. They are inconsistent, so you could have, if you had positive thyroid antibodies, you could measure them daily for three weeks, you would probably never see the same reading more than once. You could see orders of magnitude difference of them.
Part of that can be your variation, part of that can be just laboratory analysis, so many people say, “I did X. My antibodies went down. That was good. X is good. I did Y and my antibodies went up. Y is bad.” They may have done that anyway, so I just got to throw that out. There’s a whole lot of noise within this signal discussion, within that signal to noise ratio.
The counterintuitive impact of iodine
Food matters and the biggest, most-documented dietary thing that affects Hashimoto’s by far is just iodine intake. The more we consume, the worse it goes, and that’s … It’s counterintuitive, but your thyroid needs iodine so badly that when you get a lot of it, you’ve got to shut down the factory or else you’d make so much hormone you would hurt your heart.
Ari Whitten: I think this is worth going a little deeper into because it’s very counterintuitive and if someone … I think the biggest problem with it is that when someone suspects they have a thyroid problem or even when they’re diagnosed with it, they might go on Amazon.com and look up natural thyroid supplements, and almost all of those thyroid supplements that are marketed with the idea that they’re beneficial for thyroid function have iodine in them. There seems to be a pretty big disconnect there as far as the science relative to the marketing of supplements.
Dr. Alan Christianson: I think this goes back to a bigger concept, which another thing I love about your understanding is that you’ve gotten this one too, is that nutrients facilitate reactions but they’re not sufficient unto themselves for reactions. A nutrient is not something that the more of it you take, the more something happens in your body ad infinitum.
There’s always this thing like this C-shaped curve or this J-shaped curve to where the absence of a nutrient causes some negative change, and then the excess of a nutrient causes some negative change.
The lack of iodine, somewhere less than 50 or 100 micrograms we see higher rates of goiter especially, goiter in thyroid nodules.
Then the excess of iodine, somewhere above about 300 micrograms for the total day’s intake, we see higher rates of thyroid autoimmunity.
In the modern world here in America, we had, for example, in Michigan, places in the country to where there was not a lot of iodine in the soil, it was by the Great Lakes, you would see school-aged children, a third of them having goiters, literally 30, 35%.
Then along came the little Morton’s girl holding the umbrella, you know iodine fortification, and that was 1910 roughly around there. Within a decade that rate of goiter plummeted tenfold. That was cool.
Then in the following decade, Hashimoto’s came to America.
Ari Whitten: Interesting. Another question, and maybe there isn’t good enough science to answer this, but I’m curious if you think there’s anything to more like isolated iodine being added, let’s say, to supplements or to salt, for example, versus natural sources of iodine, like, let’s say seaweed. Do you think that there might be any difference in the effects on the body, or is iodine, regardless of where it comes from?
Dr. Alan Christianson: That’s how I would take it. I have seen many who have talked about different forms of it or nascent iodine or micronized iodine, but, yeah, you’re right, elements are elements, and short of a particle accelerator, we can’t change elements in any meaningful way.
Ari Whitten: Basically if I’m reading you correctly, you’re saying I should get a particle accelerator.
Dr. Alan Christianson: I’ll be happy to prescribe that and sign it off for tax purposes, as long as I can come play with it too, sometimes.
One last thing to throw in there that’s important, I think, is that that upper safe limit of 300 micrograms for those with Hashimoto’s who are prone to it, the big thing to think about also, like we talked about before, is that thyroid meds have iodine. So, if someone is being treated and they’re on thyroid medication, between that and just any amount in the diet they’re probably already up against that upper limit. In those cases, the real trick is to avoiding all the extra to improve their condition.
Ari Whitten: You would have to be mindful of even if you’re consuming Morton Salt if you’re consuming the iodized salt versus sea salt, do you think that’s a significant factor as well?
How to control iodine consumption in your daily meal
Dr. Alan Christianson: So many people that I see, I see them reverse commonly. I see antibodies go down, and one of the big things I’m adamant about is just no extra iodine.
Pretty much all [Inaudible] have that. You’re right, it’s added to the salt. There are times to where I need someone to be on a low iodine diet for purposes of testing, like nuclear uptake scans.
You’ve got to pretty much stand on your head to get below 50 micrograms. It’s not easy. You always get some.
You’ve got this basal amount, and then if you’re on thyroid medications, most potencies are at least 130 to 200 micrograms. Those two alone, you’re at this upper limit, and then every speck above that there’s just more inflammation and more trauma.
I just have people really scour, and to be precise. Probably the biggest food category to be mindful of apart from those few we mentioned like thyroid supplements or other iodine-containing supplements would be sea vegetables.
I’m a fan in other contexts, but someone who’s in that scenario, kelp, and kombu, and haziki, and arame, they can easily push them over that limit. Nori, like a sushi wrap once or twice a week, not a big deal, like maybe 30 micrograms, but other versions do get to be excessive for them.
The evidence on how grains and gluten impacts people with autoimmune diseases
Ari Whitten: Got you. Another big theme as far as nutrition and Hashimoto’s is grains and gluten, and there’s a lot of fuss around the idea that gluten or grains, in general, might cause not just celiac but autoimmune diseases of all types. What’s your general take around that?
Dr. Alan Christianson: There’s individual experience and there’s actual evidence. I’ve got friends who’ve done polls, and a large percent of people who have thyroid disease who have gone gluten free have felt it’s been helpful for them, so there’s that.
In terms of whether or not grains are part of the autoimmune cascade, there’s really no evidence saying that, and there’s actually a lot of evidence to the contrary.
We look at Mediterranean populations, we look at many populations like in South America, for example, that have had lower rates of cardiovascular disease, lower rates of diabetes, we don’t see a link between grains and actually triggering autoimmunity.
The one thing that does exist is that there is a higher rate of celiac disease amongst those that have thyroid disease, and by higher rate, I want to get exact, so most populations we see about 1% of biopsy-confirmed celiac. If you’re looking at a population of those with Hashimoto’s, that could be 3 to 5% celiac, so it’s higher. It’s not everyone.
If someone does see a big shift, there’s probably no harm to avoiding gluten, but I wouldn’t encourage complete grain avoidance. We know so much about how critical the gut flora is, and if someone does cut out intact whole grains, legumes from their diet, now they’ve gone from about 16 possible versions of fiber down to about four, so there’s a big hit in the overall diversity of the gut flora.
Ari Whitten: Interesting.
Dr. Alan Christianson: One more thing to throw in that, if you go on PubMed and if you put thyroid and gluten, you will see five studies come up, and three studies are referring to the concept that I mentioned about how there are a few more people that have celiac in the Hashimoto’s world than the other world. The other two studies are showing that if you’ve got celiac and you’re on thyroid medication, even if you’re not eating properly you’ll still absorb your medicine. That’s the sum total of all the data from research.
Ari Whitten: In other words not very much. Just for people who are not familiar with PubMed searches, five results is not a whole lot.
Dr. Alan Christianson: That’s what they say. That’s all that they’re saying. There are no other real causative factors than that.
Ari Whitten: Interesting. For people that you work with that have thyroid conditions, you, I would imagine that you obviously don’t see a huge problem with gluten or grain consumption.
Dr. Alan Christianson: I do always screen for celiac, and I do screen for food reactions. Most labs really suck for that by the way, but a few are pretty accurate. I do screen for food reactions. Most reactions that I see that are not celiac, I think about as significant, but not as something you’re stuck with like baggage. I think it’s something to work around and correct. Longer term, yes, I do like more diversity in the diet, and we see just better diversity in the gut flora and better immune response from that.
The importance of a diverse diet
Ari Whitten: What do you mean by diversity in the diet?
Dr. Alan Christianson: Covering a lot of food categories, so probably the … I could illustrate this by the opposite. I’ve seen many that have gone on extremely limited diets like they’ve heard about some of the autoimmune paleo approaches, and they’ve done not much besides greens and some versions of red meat. There seemed to be some short-term benefits for some people.
But the difficulty is that your gut is very adaptable both in terms of expanding your repertoire but also in contracting your repertoire, so if you’re eating very few foods, you become able to digest very few foods.
Then, also, there’s data saying that if you’re too low in many versions of fiber, you’re not getting prebiotics. You’re not feeding your protective flora, and then we see the whole issues of leaky gut. I’ve seen so many to where they’ve done those regimes for longer periods of time, like more than four weeks, and they get painted into a corner to where now they want to eat more foods, but everything they eat they react too badly, and that’s not a good situation.
The inaccuracy of food intolerance testing at laboratories
Ari Whitten: Interesting. I want to get into the gut stuff in a second, but there’s one more thing I want to ask you about because this is a conversation that we had on a recent trip we took together to the Grand Canyon when we went backpacking. It was absolutely fascinating for me, so I’d love for you to share this with people.
You talked about doing split testing with samples that you sent out to the food intolerance testing laboratories, and you had mentioned … I’ll let you explain it, but tell me about some of those tests that you did.
Dr. Alan Christianson: I’ve always been enamored by good, objective data, but also a little suspicious. I want data to be meaningful, and I want to know that it’s accurate for someone, and I worked in one of those laboratories quite a while back, and I knew that there were some pitfalls and some ways in which the data could not be accurate.
As a clinician, the easiest way I can gauge … One first little qualification I have a test go through is just to see if it’s reproducible, just see if that same sample of blood would yield the same results even if it came in under two different tubes with different names.
That’s a sneaky little thing that I’ve done, but has been hugely, hugely informative for me.
Ari Whitten: In what sense? What were the results? You took samples, blood samples from people. The same person, taken the same blood at the same time, and then just slapped two different names on them and sent them off to the lab. What were the results of those tests that you did?
Dr. Alan Christianson: We get two tubes of your blood and one says Ari Whitten, and one says John Doe, or something more creative than that, but not too weird. We send them in, and so you and John have completely different findings, like no relationship whatsoever.
Ari Whitten: Wow.
Dr. Alan Christianson: Once I see that, I know that this is just random noise. This is not valid information.
Ari Whitten: This is we’re talking about IGG food intolerance testing, right?
Dr. Alan Christianson: Yeah. Most will do IGG. Some will also include IGE or IGA, but IGG is the central part about food intolerance testing.
Ari Whitten: Is basically all of that food intolerance testing just invalid? Is any of it legitimate?
Dr. Alan Christianson: I’ve tested probably about three dozen different laboratories, and I have found three that have passed those tests repeatedly.
Ari Whitten: Interesting. Do you want to give the names of the ones that passed? Do you have recommendations on it?
Dr. Alan Christianson: Sure. I’m not financially tied to them. One is not currently in operation. One is US Biotech, and one is Meridian Valley. Those are ones that are reproducible data at least.
Ari Whitten: Why would that be? I guess that still leads to the question are the results valid. We know that they’re consistently getting a certain finding.
Dr. Alan Christianson: You’re right.
Ari Whitten: That doesn’t necessarily mean that …
Dr. Alan Christianson: That’s just one criterion.
Ari Whitten: Yeah. That doesn’t necessarily mean that it actually means that you are intolerant to those foods.
Dr. Alan Christianson: You know that if it’s not consistent that there’s no point in taking any further, but if it is consistent, there’s still more to think about.
Ari Whitten: Yeah. There’s still a question of whether it means anything.
Why eggs, dairy, and gluten often are causing immunologic response
Dr. Alan Christianson: Right. Clinically, I would argue that it can when it’s accurate, and that it’s something that really can evolve. There are those who have digestive symptoms.
The big three patterns we see a lot in the accurate ones are really gluten, eggs, and dairy. There are bindings to keep proteins that hold those particular things together, so you make muffins, you need some flour, and some milk, and some eggs so it holds together and coagulates.
On a micro level those are all proteins that are very complex, tightly wound batches, chains of amino acids. When they’re not completely cleaved apart, the undigested fragments they can trigger an immunologic response, and a common thing I’ll do clinically is with those results I’ll take someone and say, “Hey, just cut these foods out completely for three weeks.”
Probably 95% of the time they’ll look back and they say, “Oh, wow. I wasn’t noticing anything on a day-to-day basis, but after the fact, yes, now I don’t have bloating right now. I’ve dropped five, seven pounds of fluid, or now I have less joint pain,” or whatnot.
It can be clinically relevant, and also just one more piece about reversing the whole autoimmune cascade and lowering antibodies.
When the food intolerance test results uncover more than eggs, dairy, and gluten
Ari Whitten: Yeah. Interesting. Are you saying that that would occur just in general through asking someone to get rid of gluten, dairy, and eggs, or is that specifically you’re saying, “Here’s your IGG test, and we’re going to get rid of everything that this test says that you’re intolerant to.”
Dr. Alan Christianson: Clinically I do prefer to test because those three are prevalent, but they’re not universal, and there are times to where you can see some rather unexpected food for a given person.
The other approach is the whole avoidance, reintroduction, and it’s actually not very scientific. The drawback is kind of like the issue I mentioned with the extreme restrictive diets.
If you narrow your diet down a lot, everything inside of you gets lazy, and so now you eat a different food, and you may have done fine with that food under typical circumstances, but because you’ve been exposed to so few foods, now it may be more of a challenge.
I’ve seen many do the elimination diets where they’re consuming nothing but lamb or rice, for example, for a couple of weeks, and adding back foods one at a time and everything makes them sick. Now they’re boxed into that corner again, but it may not have been a real response in a different scenario.
Ari Whitten: Interesting. On a side note, on a more personal note, I actually noticed that I developed a food allergy recently and it’s to dairy. That kind of annoyed me because dairy has been a big part of my diet for a long time, and I’ve never had any negative reaction to it up until about a year ago.
I started to notice actually that I was waking up with a little stuffiness, and kind of an irritation in the back of my throat, which I thought was I was getting … I thought I was getting sick. It kind of has that feeling like at the beginning of when you catch a cold. I thought that’s what it was, and then it went on for like a week, two weeks, three weeks, four weeks, and I never actually got sick. Then I started to think maybe it was seasonal allergies or something like that which I’d never had, as well.
Eventually, I just had the thought to try and remove dairy from my diet, so I removed all sources of dairy. These symptoms that I’d had for many months cleared up within about a week, and then I went back to dairy to try again after about three weeks of removing it, and sure enough, I had symptoms pretty instantly. Got very congested and started waking up again with that kind of stuffiness and irritation in the throat.
Very odd to me that I would just develop an allergy out of nowhere after so many years of consuming it. I don’t know if you have any insights into how allergies actually develop or emerge randomly.
Dr. Alan Christianson: To be really nuanced, we do distinguish allergies and intolerances and sensitivities. Things in this category can evolve both ways. They can show up and they can come and go, and sometimes there are not apparent symptoms that people have to be aware of as far as them being ongoing immune stressors. Any big shift in the flora can be responsible for that, any reason the gut flora can change, which can be numerous, so that does happen.
The relationship between leaky gut and gut permeability and the generation of autoimmune conditions and Hashimoto’s
Ari Whitten: Interesting. Let’s get into the gut stuff. Is there a relationship, I guess, first of all between leaky gut and gut permeability and the generation of autoimmune conditions and Hashimoto’s in particular?
Dr. Alan Christianson: There’s a relationship for sure. It’s not universal. It’s not behind everyone’s case of Hashimoto’s, and I think that’s an illustrative concept too, is that there are these things that have been thought of as root causes or trigger factors, but kind of like the symptoms, they’re not the same for all people. Not everyone has the same total load of immune stressors.
There’s some core genetic susceptibility to develop thyroid disease, and that actually affects the iodine transport mechanisms. Some people have very selective iodine transport where it just gets iodine. Others it’s less selective, and they’ll pull in a larger number of wastes.
You’ve got that transport. You’ve got the exposure to various wastes that could accumulate in the gland, then you’ve got the sum total of immune stressors.
And so, a lot of different things could fit in those categories, but for many that immune stressor certainly can be related to the gut health, and there can be this combination of foods they’re reactive to and the state of their flora, and it’s hard to say which is the chicken and which is the egg because it can go either direction.
Consuming foods that you’re sensitive to can harm your flora, and then having a compromised flora can make you more reactive to more foods. It’s often a matter of not knowing which is the ultimate cause but just addressing both, really assessing both and taking care of both. It can be part of the causative factor for some people.
What it means to take care of your gut
Ari Whitten: What does that mean, to take care of your gut? There’s a lot of gut issues that are happening right now to a lot of people, like, for example, SIBO and leaky gut. These are kind of hot terms that a lot of people are talking about right now, and a lot of people seem to be suffering from. How do those conditions actually come about?
Dr. Alan Christianson: SIBO is an overgrowth of good bacteria, and that can be also from alterations in breakdown of proteins, that can be from chronic antibiotic overuse. That can also be from probiotics, believe it or not. That can be a source of SIBO for some people.
Leaky gut, similar factors: compromises in the flora, also some are just more genetically susceptible to it. It’s also common and secondary to some version of an inflammatory bowel disease or irritable bowel syndrome, so it can occur.
I think there are many instances in which people can read about symptoms, very broad, vague symptoms of these conditions, and then assume they have them, and then do various efforts and hope they got better.
I love to know for certain, and they’re very testable things, so whenever there are concerns about autoimmunity, those things are all measurable. You can see if you have them or not, and the other beauty about a good diagnosis is that you can see if they get better or not and if your efforts were effective. If they did resolve you can just take that particular cause and let go of it, and perhaps screen in the future, but know it’s not an ongoing factor for you.
Ari Whitten: Interesting. As far as SIBO or SIBO. I don’t know if there’s a technically correct pronunciation of it.
Dr. Alan Christianson: I’m sure not. I hear SIBO a little more common.
How to treat SIBO
Ari Whitten: We’ll go with SIBO. What do you recommend as far as a way of treating that? If someone suspects they might have it, what would a treatment typically look like?
Dr. Alan Christianson: I would go further and then test because there are different versions of that. There’s some to where there’s more hydrogen output, some where there’s more methane output, and those point towards different strains of bacteria primarily.
Treatment, there’s some conventional treatments that are rather effective. They can be costly, and they can cause … They can still have recurrence, so Xifaxan is one of the main antibiotics used. I’m such an avoidant doctor from not using antibiotics, but there are some medications that are in different categories. We think of like a topical medicine, you put that on your skin.
Your gut, if you imagine you’ve got a tube that’s this big from your mouth to butt, and you drop something in that tube, it’s going to bounce on through and have no bearing upon your chemistry. It’s not in your body. It’s really outside of your body when it’s in that tube, so your gut is actually like that. It’s just a lot longer and a lot skinnier.
A medication that you take but you don’t absorb is considered topical. Xifaxan is actually a topical medicine oddly enough. You consume it and it works through the intestinal tract, but it’s not coming into your liver or your kidneys, your bloodstream, or elsewhere in your body.
The idea about systemic side effects is not really plausible. Not many medications are like that. Nystatin’s one of the few others, but there are some that are actually oral topical.
Ari Whitten: Interesting. I’ve never heard of that before.
Dr. Alan Christianson: Yeah. Curious concept. Pretty good margin of safety. High-cost factor. There are many times to where people can have some level of coverage for that, or the manufacturer can give discounts when it’s requested or whatnot.
It’s one of the more successful mainstay treatments for both versions of SIBO.
The consideration is just the recurrence risk, and by and large, if someone does have good analysis of their gut function and their gut flora and appropriate steps to remedy those, that goes a long ways towards cutting that risk of recurrence after treatment’s over.
There are also a lot of non-conventional treatments that have used berberine and various delayed-release essential oils or gum mastic or some extracts from artemisia that have had some level of efficacy as well.
It’s a treatable thing, but it’s really a matter of not just killing the overgrowth of those bacteria because they’re good bacteria. It’s normal, healthy bacteria that there’s too many of, so it’s really getting the extra ones down, but then changing whatever factor was lacking that allowed them to overgrow.
Why low carb diet is one of the easiest ways to leaky gut
Ari Whitten: Got you. Talk to me a little about leaky gut, and I know that you had … You’d went into this a bit, and then I backtracked into more diet stuff, but you talked a little about fibers and the relationship of that with leaky gut. How do they relate?
Dr. Alan Christianson: Odd thing is one of the easiest ways you can induce leaky gut is to go really low carb. Lots of evidence on that.
Ari Whitten: Why is that?
Dr. Alan Christianson: You’re starving your bacteria, so not only fibers but actual carbs are prebiotics. They’re fuel for the bacteria, and the funny thing is that there’s a lot of thought about flora and bacteria, and people’s minds go right to probiotics. The disconnect there is that 99% of our flora is anaerobic. They live in an oxygen-starved environment. There’s no sunshine in there. It’s a dark, airless place.
Ari Whitten: Hence the expression: where there ain’t no sunshine.
Dr. Alan Christianson: Where the sun don’t shine.
Ari Whitten: Where the sun don’t shine. Yeah. Thank you.
Dr. Alan Christianson: Think about it that way. There’s no oxygen, no sunlight, and they’re in a whole different ecosystem. Probiotics, they’re aerobic organisms. They’re ones that live in an oxygen-based environment. They’re the tiniest little minority of our gut flora.
You can take all the pills you want, but you’re not affecting 99% of your flora. You only affect them by feeding them, and they’re fed off of carbohydrate and carbohydrate remnants: fibers and probably resistant fiber is the best documented, but there are really many versions of fiber, and they do best to get a good variety.
The truth about carbohydrates disrupting the gut microbe
Ari Whitten: There are a couple of things here. One is carbs and feeding the gut microbiome because sometimes you’ll hear people talk about eating too many carbs as disrupting the gut microbiome. Can you clarify that? Where do carbs or maybe certain kinds of carbs start to disrupt the gut microbiome and where are they beneficial?
Dr. Alan Christianson: This is the illustrative point. It’s a good question. Carbs can be factors. I’ve heard people talk about this in terms of water on a plant. If you’ve already got weeds growing and your lawn is totally bone dry, you can kill the weeds, but at the same time, you want to have water on your lawn.
Yes, you can starve the gut of carbohydrate, and you can inhibit the growth of certain types of bacteria, but you’re not really allowing the growth of the others. It’s true for bacteria, it’s also true for fungi that if they’re already overgrown and they’re pathogenic, yes, carbs can fuel that the same way that water can fuel weeds.
In the absence of carbs, you can just starve everything, but that’s not … You won’t get a good lawn out of the deal, and that’s in that same regard.
They’re not the cause of it per se, but they, no more than the way that water is the ultimate cause of weeds.
The effect of resistant fiber on leaky gut
Ari Whitten: Got you. The terrain is really important here, and what kind of soil you’re providing, I guess you could say, to the different microbes that are growing there. You mentioned resistant fiber in there. I know that this is something that you’ve written about before. Can you just talk a bit more about maybe the links between resistant fiber in particular, and how that affects leaky gut?
Dr. Alan Christianson: Pretty exciting, so the bacteria in our gut, they make various chemicals that are good for us or indifferent, or harmful to us. One of the more salutary things we see is butyric acid or butyrate, and there are strong amounts of data saying that that helps to repair the colon lining, the epithelium, so reverses leaky gut.
It’s also a big thing cutting the risk of colorectal cancer. Butyrate, people think about butter. You get just tiny speck amounts in butter, but you make thousands of times greater quantities by your flora and the strongest …
Ari Whitten: Sorry, but what if I add many, many tablespoons a day of butter to my diet? Then will I get enough butyric acid then?
Dr. Alan Christianson: You can get up to a couple of milligrams of that, but your flora can crank out dozens and dozens of grams of it.
Ari Whitten: Are you saying I shouldn’t have many tablespoons of butter every day?
Dr. Alan Christianson: You’d probably need about 18 gallons or so to get a therapeutic dose.
Ari Whitten: All right, I’m on it. Resistant fiber.
Dr. Alan Christianson: Resistant fiber, AKA resistant starch, pretty unique molecule, and it’s a category of molecules, but carbohydrate is about four to five calories per gram and digestible mostly by the small intestine, and we use various compounds, various hormones to control its rate of entry into the bloodstream, so insulin and glucagon.
Fiber on the opposite side of that, no calories, absorbed anywhere and mostly acting in the small intestine and the large intestine. The resistant fiber is right in between the two of those.
It’s about two calories per gram and it does yield energy to us, but it’s only yielding energy from being metabolized by the bacteria in the colon, so because of that, it’s taking … It’s like a time release type thing. It’s taking three hours or so to even start producing energy, whereas regular carbohydrate can act in a matter of minutes.
You end up with about three to nine hours of stable and steady blood sugar from that, and it’s also a direct fuel that your gut flora makes into butyrate and other beneficial short-chain fatty acids.
What the best food sources are for resistant starch
Ari Whitten: Got you. Very interesting. Where do I get resistant starch or resistant fiber?
Dr. Alan Christianson: Your best commonly available food sources would be white beans: navy, northern, Cannellini, or potatoes. Potatoes, the cool thing is that the more times they’re … First, you want to boil them, but then after that the more times they’re heated and cooled, the more amount of resistant starch you’ll get from them.
Ari Whitten: Won’t potatoes give me diabetes? I know that’s a topic …
Dr. Alan Christianson: You got me there.
Ari Whitten: … of your passion. I know I’m kind of opening up a very deep discussion, in that we could probably talk for an hour on that topic alone. The point for anyone listening basically …
Dr. Alan Christianson: Anyone listening please read the Low Carb Myth. You’ve got to go through the book, seriously, and look at all the science and all the explanations. That’s the proper answer.
Ari Whitten: Yeah. I guess we’ll save it for that. He just gave you a pitch for one of my books, so we’ll leave it at that.
Detoxification. I guess I think it would be helpful to jump out to the big picture for a moment and just talk about … We’ve talked about a number of factors that can contribute to thyroid conditions. We’ve talked about a number of things that can be helpful. We’ve talked about a number of things that are not necessarily helpful and are maybe more based on fads and pseudo-science.
The most significant causes of Hashimoto’s
As a big-picture overview, what do you think are the most significant causes of why somebody would get Hashimoto’s in the first place?
Dr. Alan Christianson: There’s that triad, that perfect storm of genetic susceptibility, toxicants from the environment, and then stressors of the immune system. The toxicants are very well documented in the case of Hashimoto’s. Ironically, iodine is the best-documented toxicant, but there’s upwards of 300 other chemicals that have been shown to be highly associated with it. That’s the big factor.
Ari Whitten: That was an interesting statement. Iodine is a toxicant, but I’ve never heard of it described in that way. Normally it’s described as an essential nutrient for health or thyroid health in particular, so can you clarify a little on that?
Dr. Alan Christianson: It’s a fascinating thing. It’s probably the most studied nutrient on the planet by far.
I talked about how we added it to our salt. They’ve done that all around the world with varying degrees of proper performance and controlled outcomes, and it’s created a lot of unintentional experiments so to speak. We’ve got large amounts of data on how populations respond to varying changes of iodine intake, and sometimes unintentional. We’ve been backpacking. There are times where it’s been used as a water purification source, and that’s also created some unintentional experiments, so to speak.
One of the easiest ways to induce Hashimoto’s disease is to have a consistent overdose of iodine.
Ari Whitten: Interesting. You mentioned a lot of different toxins are documented to contribute to thyroid conditions, so let’s go … Iodine is covered. Let’s talk about some of the other ones.
Why Teflon is a cause of thyroid disease
Dr. Alan Christianson: The big ones that come up are perchlorate, lead, mercury, Teflon, many, many others from there on down, but they’re some of the top few. Actually, fluoride is up in that list also.
Ari Whitten: Interesting. Is Teflon actually … Has there been science that has linked it to thyroid conditions?
Dr. Alan Christianson: There has been, yeah.
Ari Whitten: Interesting.
Dr. Alan Christianson: Some of the derivatives formed from that’s subjected to high heat, so the older Teflon pans in theory if they were never scratched at all or subjected to too high of heat, probably quite safe, but in the real world they get hot, they get little microscopic nicks in them, and they have been shown to be correlationally associated with the onset of thyroid disease.
Why fluoride is a direct factor of thyroid disease
Ari Whitten: Interesting. I didn’t know that. Some of these other toxins, for fluoride. I know that fluoride from what I understand is often … It can be used to actually treat hyperthyroidism, can’t it?
Dr. Alan Christianson: That’s why. Back before we had our current generation of medications for hyperthyroidism, fluoride was one of the mainstays of treatment.
Fluoride, it’s close enough to iodine to where it takes hold in the iodine receptors and just fills them up, so the body is less able to assimilate iodine within the thyroid, so you can create a net severe iodine deficiency and something like a blockade or a siege so to speak by a high enough continual dose of fluoride.
That’s been most relevant in areas that have fluoridated water. That’s been shown to be a direct factor for Hashimoto’s, but also thyroid cancer.
Ari Whitten: Now, is that just a US thing that people need to be aware of, or do other countries also fluoridate their water?
Dr. Alan Christianson: To be honest, I don’t know either way.
Ari Whitten: I was hoping you know because I didn’t know.
Dr. Alan Christianson: I’m sure Doctor Google knows that one, but I don’t know that.
What to do to minimize exposure to toxins
Ari Whitten: What do you recommend as far as … I guess, having said that there are all these different toxins, and I’m sure we could go into a deep dive discussion on probably a couple of dozen of them, but do you have any broad recommendations for minimizing exposure to some of these more important toxins?
Dr. Alan Christianson: I heard a pretty fascinating one from a doctor recently. Yeah, get married. Believe it or not, that’s well documented to lower your toxic burden pretty substantially.
Ari Whitten: How does that work?
Dr. Alan Christianson: It’s probably a matter of eating at home more than eating out.
Ari Whitten: If you’re a single male, you’re going to eat a lot of fast food and a lot of junk, and by getting a wife she’ll make you some good home food.
Dr. Alan Christianson: Probably the biggest factor there is your food containers, is just your plastic exposure, your cumulative plastic exposure, so minimizing your plastic burden would be a huge step.
Ari Whitten: Glass containers, glass bottles, things like that.
Dr. Alan Christianson: Yeah. My favorite thing back when I was in my late teens, I worked in a food cooperative. These things were so counterculture back then. It was so not mainstream to be into organic foods or whatnot, but all of the loyal adherents to our coop, they would come in with their glass jars that had the tear weight pre-labeled, so we knew what the jar weighed, and they went to the bulk containers and they filled up and got their beans, their legumes, their nut butters, their oils, or whatever else it was, and came in and weighed them in their own containers.
They already had fabric bags. There was just no garbage, no waste, no plastic that was any part of the transaction. Again, it was so weird. It was so counterculture, and weird, and hippy, but it was brilliant. It was really the ideal way to go about those things.
How to minimize fluoride exposure
Ari Whitten: Yeah. For sure. You mentioned fluoride. Did you have any recommendations on minimizing fluoride exposure?
Dr. Alan Christianson: I’ve never seen data suggesting that normal fluoride use in dentistry is relevant, so fluoride treatments or fluoride seals or whatnot don’t seem to be a factor, but really day-to-day fluoridated water could be a problem for that and other reasons. Also, I’ve seen links to stomach cancer.
There are many reasons why tap water’s just not a good option, so you really want purified water for your daily drinking purposes.
Ari Whitten: Is there a particular filter technology that you’d recommend above others or just filter?
Dr. Alan Christianson: I’m a fan of reverse osmosis, and that’s a level of technology that’s pretty easily attainable and yields a clean, pure product.
How cortisol is affected by your daily rhythm and HPA Axis
Ari Whitten: Nice. Talk to me a little about daily rhythms and I know we’re going to try and wrap up here in the next 10 or 15 minutes or so, but can you talk a little about daily rhythms of cortisol and the HPA axis and why those are significant?
Dr. Alan Christianson: For sure, so back to that model of onset with susceptible genes and then also the toxicant exposure and then immune stressors, the daily rhythms affects the first and the third part of that, so your gene expression is highly conditional upon this cortisol cycle your body goes through, as is your immune defenses especially.
In a perfect scenario, we make this cortisol spike that it’s like our internal coffee machine. It wakes us up. We’re alert. We don’t want to stay in bed. We want to get up and do things, and then as we wind our way through the day it shuts down, and the parallel version of the nighttime hormones comes on as cortisol goes down.
As cortisol plummets, melatonin creeps up. We get this nice melatonin peak. We’re exhausted. We sleep like a baby and wake up well refreshed. That’s the ideal scenario, and it’s crazy when I wrote the Adrenal Reset Diet Book I was looking at just how many facets of our body’s chemistry was conditional upon that cortisol rhythm.
There was almost nothing I could find that wasn’t. That circadian rhythm is affecting just every process across the board, but a lot of data about it affecting the immune response, so how well you can ward off chronic infections, how well you can maintain resistance against early cancer cell growth, but very relevant as far as a source of immune stress.
Ari Whitten: What kinds of things are affecting that rhythm of cortisol and the HPA axis? I guess for those who are not familiar with the terminology, HPA stands for hypothalamic pituitary adrenal.
Dr. Alan Christianson: Yeah. Factors that affect that are just quite simply modern life, like everything in modern life, like living inside, being disconnected from actual sunlight, and not sunlight through windows but actual direct exposure to sunlight, being separated from temperature changes that are throughout the day cycle and throughout seasonal cycles, being indoors and physically constrained, not physically responding to our stressors, but mentally only responding to our stressors, all these factors and more disrupt that cycle.
What you need to do to normalize your HPA Axis
Ari Whitten: Interesting. As far as the relevancy of that to treatment in the course of, let’s say, treating somebody with Hashimoto’s or treating somebody suffering from fatigue, what kinds of things are helpful to help normalize that HPA axis rhythm?
Dr. Alan Christianson: One thing that I talked about which is a simple strategy is the timing of carbohydrate. Carbohydrate via its effects upon insulin has a property of lowering cortisol output, so if you have your days allotment that’s more so backloaded to where more of that’s later in the day, that can help make like a trellis almost for a plant where that rhythm comes back and improves itself again.
That’s a simple strategy that I’ve shown can help regardless of other variables. Other factors are really thinking about those things that disrupt it and stopping as many of them as you can, so getting yourself exposed to good daylight when you wake up and avoiding exposure to electronics in the evening, being colder at nighttime intentionally, letting your body be at a cooler level, maintaining regular physical activity and avoiding long prolonged periods of immobility.
Back to the toxicants again, there’s also data saying that these things independently act upon our stress control pathways. Carrying lead in your body is just like having … is like living in an unsafe neighborhood as far as how it affects your cortisol metabolism, so also detoxing benefits that part as well.
Ari Whitten: Now, have you seen through detoxing people, getting rid of let’s say a lead build up or mercury build up or any of these different chemicals we’ve talked about, have you seen people’s cortisol and HPA axis function normalize as a result of doing that?
Dr. Alan Christianson: I have, and kind of like the early discussion about the root causes being different from person to person, when I screen someone and their environmental burden is minimal, then that’s not a big lever for them. That’s not going to be a big game changer for them for much of anything. They’re probably fine already.
Some people have had less exposure than others but some people are more Teflon and some are more Velcro. Some people whatever they’re exposed to will not build up. Others are the opposite, more things stay inside of them. People have different levels of toxic burden. When someone has a very substantial toxic burden, then I’m very confident this is going to be a game changer for them in many ways.
Dr. Christianson’s take on chronic infections
Ari Whitten: Cool. Last question. This is maybe a big one, but what do you think about chronic infections? I know that there’s a lot of fuss right now over this idea of chronic infections, stealth infections, hidden infections. Probably the next term is going to be ninja infections. Then I’ve heard people talk about this and this is a very old idea in the naturopathic community.
I know that even Joseph Pizzorno in his recent book, The Toxin Solution, made reference to this idea of chronic infections and said it’s been around since, like I don’t know, the 70s in the naturopathic community and people have been talking about that, and then I think it kind of went away for a period of time, and now it’s kind of come back. What’s your general take on this idea of chronic infections?
Dr. Alan Christianson: It’s relevant, but like all things, again, it’s relevant for some people more than others. It’s not a universal cause. The drawback about these cycles or these, I don’t know, fad is too derogatory of a term, but these things that become more in vogue for periods of time is that you can look at vague symptoms and be sure you have something, and take various steps and perhaps feel better, but not be certain about that, and not really know what the outcome was, so it’s always good to test and don’t guess.
The big picture is that there are so many organisms that share a ride with our bodies, and a few of them were actually really helpful for us. Most are just along for the ride and some are harmful given the right circumstances.
If your body is compromised in some way, there can be this escalating cycle to where your weakened immune response allows some bad bugs to become more active than not, and they can, in turn, create various metabolites and byproducts that further weaken the immune response.
There’s a slippery slope in which immunocompromise can lead to opportunistic infections and further immunocompromise, and we see dramatic examples of that in hospitalized patients, like HIV or chemotherapy or other examples of clear immunosuppression. To some extent that can happen and probably the gut is one of the larger reservoirs of that, the gut and then also the blood and the lymphatic system for chronic viruses, so it can happen.
What the common infections that are linked with Hashimoto’s are
Ari Whitten: Interesting. Are there any infections in particular that you’ve seen that are linked with either, let’s say, fatigue or linked with Hashimoto’s in particular?
Dr. Alan Christianson: As far as gut infections numerous are possible. We can see overgrowth of more fungal organisms: geotrichum, candida, many others. Scores of possible bacteria infections, also the deficit of good bacteria can look similar, and multicellular parasites can occur.
Then bloodborne, most commonly we’re seeing there are herpes-type viruses, so Epstein-Barr virus, HHV-6, cytomegalovirus. Those are all ones that we think about especially if someone just gets colds and flus’ way too often, if they’ve got ongoing swollen nodes for no clear reason, unexplained fevers, maybe they were never well since they had mono when they were in college. Those things can happen.
The three most important things that Alan wants you to know if you have or suspect you have a thyroid condition
Ari Whitten: Interesting. To wrap up, if there are, I guess, maybe three things that you want to leave in people’s minds as being really of great importance for them to either get checked out or for them to think about addressing if they have a thyroid condition or suspect they might.
Dr. Alan Christianson: The most important three things…
#1 You can get better
I think, the very first one is I’ve never seen anyone that couldn’t get better. By get better, I wouldn’t define that as the absence of thyroid medication, but I would define that as the absence of thyroid symptoms.
I’ve seen many people get better as in reaching a state of having the absence of thyroid medication, but the most important thing is living well and enjoying your life.
Probably throughout the course of our lifespan, there’s going to be some mixture of pills we take, and we change those over time, but we’re probably never not going to take any pills at all. That’s not the biggest outcome in life is to have this pill gone and that pill here. I mean who cares? You’re functioning. You’re doing well. The biggest goal is really getting past those symptoms.
It’s possible. People can do that. Even further than that, I would argue that when you’ve gone that deep and thought that hard about what’s affecting you, not only can you reverse the things that went wrong, you’re going to come out better than you were beforehand. There’s a lot of things that may not have been ideal that weren’t bad enough to have gotten your attention before, so on the other side, you come out even better than you were beforehand. That’s a big one.
#2 Know what your unique causes are
The other one is that it’s important to know what your unique causes, your unique triggers are and they’re not the same as everyone else’s.
#3 Track your progress
Not to get caught up on thinking that you’ve got to have this latest thing and that it’ll never go away, but, no, just have a good relationship with a solid practitioner, and do some thorough screening to know what your biggest culprits are, and once you know what those are, then the third big part is just track them.
Do some reasonable steps for a period of time and recheck did that clear up? Yes? Bonus. No? Okay, we’ll try harder. We’ll look again. That’s really the mindset, just knowing what it is that’s affecting you and how you can reverse that and then confirming that it did occur.
Dr. Christianson shares details about his new thyroid program
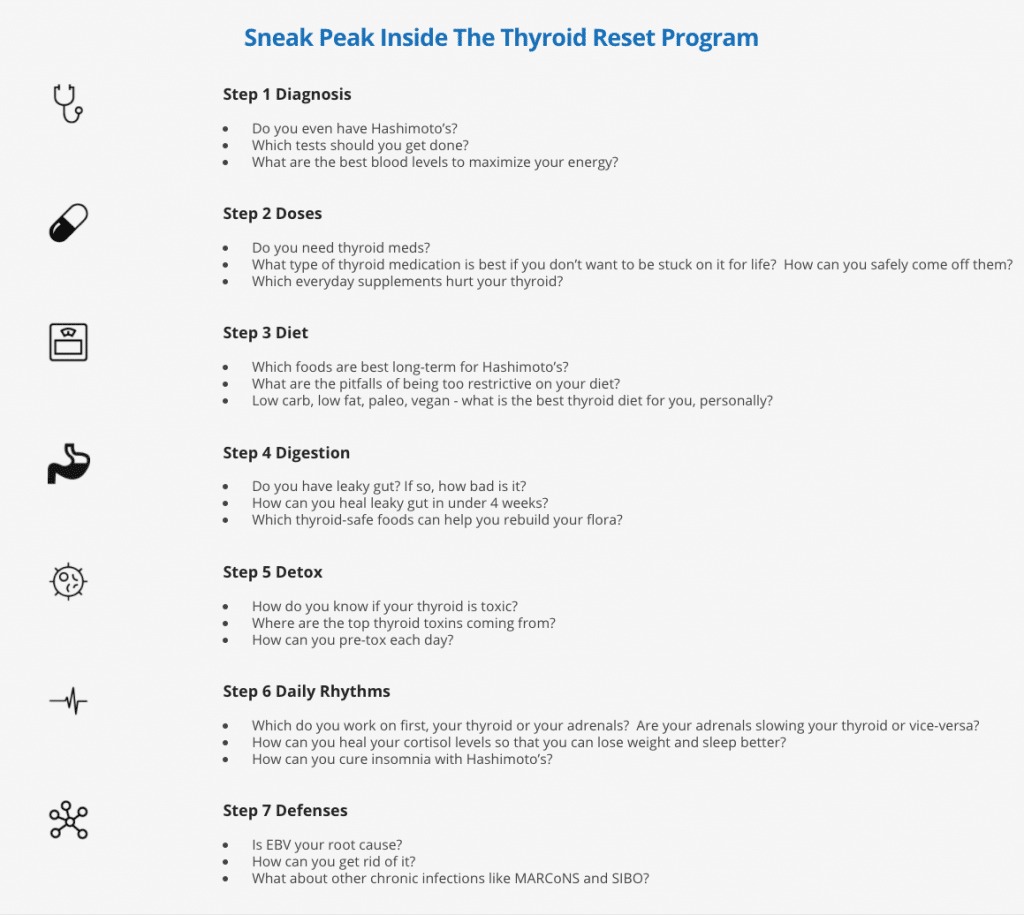
Ari Whitten: Beautiful. On one final note, I know that you are releasing a thyroid program. I know that you’ve had a thyroid program around for quite a long time, and I think you have done a bunch of recent updates to it or completely redid the course. Tell me a little bit about what you did there.
Dr. Alan Christianson: Completely redid it, and I had a great one that thousands of people have gone through and had good results from. I kept at those core ideas, but I just made it all from scratch, and I reached out to my subscribers and I asked them, I said, “Hey, what are some things you’ve really been stuck with? What are the things holding you back?” In a matter of hours, I got like 250 very articulate and very thorough responses. I was just so touched and
I went through them just like you’d read scripture, I mean like just word for word, and, okay, I’m not going to miss this. I’m going to cover these bases. I totally redid it to cover all these things. I use this process of the seven D frameworks, you mentioned some of those, about: the diagnosis, the dosages of medications or supplements, the diet, the digestion, the detox, the daily rhythms, the defenses.
There’s really a step process because the first things you do well often negate a lot of downstream steps. That’s the cool thing about working with bodies versus cars is that if a car’s got a bad radio and bald tires, you don’t get better tires by fixing the radio. In the case of a body if you’ve got multiple issues, if you solve something upstream, you will resolve many things downstream.
The sequence is all done to where it’s as easy as possible. You take care of the biggest things first and manage small brush fires if they’re even still there or not.
Ari Whitten: I guess that works in both directions with the body. When one system dysfunctions, other systems can dysfunction, and you’re talking about …
What the 7 D’s are
Dr. Alan Christianson: They do. There’s a certain hierarchy to that, so when you look at the ones that are the most core and the most central, then you can resolve the greatest number of issues from the fewest number of steps.
Ari Whitten: That’s beautiful. You’re just talking about switching it from a downward spiral to a positive, upward spiral.
Dr. Alan Christianson: That’s right.
Ari Whitten: I love it. The seven D’s are diagnosis.
Dr. Alan Christianson: Mm-hmm (affirmative). Diagnosis, doses, diet, digestion, detox, daily rhythms, and defenses.
Ari Whitten: Beautiful, and so those are the seven steps of your program.
Dr. Alan Christianson: Daily rhythms, that’s all adrenal, circadian, cortisol. Had to make it a D somehow.
Ari Whitten: That’s true, otherwise it’s like D, D, D, D, D, H, D.
Dr. Alan Christianson: That’s right.
Ari Whitten: Awesome. For anybody out there who has a diagnosed thyroid condition, hypothyroidism, Hashimoto’s, whatever you’ve been diagnosed with. Now, would this also work for Graves’ or would you say that this is more specifically for Hashimoto’s?
Dr. Alan Christianson: It is more specific for Hashimoto’s. I do have a separate program for Graves’, but this is more specific for Hashimoto’s.
Ari Whitten: Okay. For anyone who has Hashimoto’s or has been diagnosed with hypothyroidism, I highly, highly, highly recommend going to check out Alan’s program. As you can tell from this interview, and I can verify because I’ve had a lot of conversations with Alan, he is the real deal.
He is, like I said, a leading thinker and a thought leader in this area, and really knows the science pretty much better than anyone that I’ve known. Highly, highly recommend him. Alan, do you want to say any final words?
Dr. Alan Christianson: Again, the big closing is that you can get better. Don’t assume you’re ever stuck with symptoms. Your body’s this beautiful homeostatic mechanism that wants to thrive.
Ari Whitten: Beautiful. On that note, we’ll leave it there. Thank you so much. Doctor Dr. Alan Christianson, it’s been a pleasure and an honor interviewing you, and thank you for sharing your brilliance with my audience.
Dr. Alan Christianson: Always fun to see you, Ari. Thank you.
Ari Whitten: Yeah. Awesome, man. Thanks so much.
Dr. Alan Christianson: My pleasure.
7 Steps To The Ultimate Thyroid Fix – Show Notes
How to know when you have a thyroid condition (5:04)
How 40% of people with Hashimoto’s are at risk of misdiagnosis (8:17)
What the different categories of diagnosis are (9:17)
Why a biopsy will not rule out Hashimoto’s (10:17)
How Hashimoto’s is a presumed clinical diagnosis (10:52)
What the optimal reference range on thyroid hormone tests is (11:44)
The standardized thyroid hormone medication (15:10)
Dr. Christianson’s preferred thyroid medication (19:02)
How conventional practitioners ignore diet as part of Hashimoto’s treatment (21:44)
The inconsistency of thyroid antibodies (22:47)
The counterintuitive impact of iodine (23:54)
How to control iodine consumption in your daily meals (26:26)
The evidence on how grains and gluten impacts people with autoimmune diseases (28:54)
The importance of a diverse diet (31:59)
The inaccuracy of food intolerance testing at laboratories (33:12)
Why eggs, dairy, and gluten often are causing immunologic response (35:55)
When the food intolerance test results uncover more than eggs, dairy, and gluten (37:05)
The relationship between leaky gut and gut permeability and the generation of autoimmune conditions and Hashimoto’s (40:11)
What it means to take care of your gut (41:37)
How to treat SIBO (43:16)
Why low carb diet is one of the easiest ways to leaky gut (45:57)
The truth about carbohydrates disrupting the gut microbe (47:35)
The effect of resistant fiber on leaky gut (48:53)
What the best food sources are for resistant starch (51:30)
The most significant causes of Hashimoto’s (52:32)
Why Teflon is a cause of thyroid disease (54:36)
Why fluoride is a direct factor of thyroid disease (55:17)
What to do to minimize exposure to toxins (56:18)
How to minimize fluoride exposure (58:07)
How cortisol is affected by your daily rhythm and HPA Axis (58:52)
What you need to do to normalize your HPA Axis (01:01:09)
Dr. Christianson’s take on chronic infections (01:04:29)
What the common infections that are linked with Hashimoto’s are (01:05:36)
The three most important things that Alan wants you to know if you have or suspect you have a thyroid condition (01:06:27)
#1 You can get better (01:06:37)
#2 Know what your unique causes are (01:07:54)
#3 Track your progress (01:08:16)
Dr. Christianson shares details about his new thyroid program (01:08:36)
What the 7 D’s are (01:10:43)
Dr. Cs’ new Thyroid Reset Program
Note from Ari: For any of you with hypothyroidism, I want to mention that Dr. Chrisitianson just released his completely revamped Thyroid Reset Program. He did just re-did the entire program and it’s packed with the latest and greatest science on optimizing your thyroid health and reversing the symptoms of hypothyroidism. What exactly does your thyroid affect? Weight. Hair. Energy. Healing. Autoimmune. Dementia. Heart health…. The list is long. LIFE long. If you have hypothyroidism, this is a must-have program. (Dr. C has also made it incredibly low-cost, so it’s affordable by everyone). You can grab it here.
Below are a few case studies Dr. Christianson wanted to share about people who have gone through his Thyroid Reset Program.
Case study 1
‘Anne’ signed up for the program hoping to lose 25 pounds and stop her progressive hair loss. No matter how strictly she dieted, her weight did not budge. Her hair loss kept going even though she hoped her biotin would help. Her current diet was strict autoimmune paleo with no nightshades, legumes, or dietary goitrogens.
At age 53, Anne started thyroid treatment about five years ago. When she started the program she was taking:
- Levothyroxine 100 mcg
- Thyroid support supplement with 200 mcg iodine
- Biotin 5000 mcg
Her blood tests were last done just a few weeks before starting the program. She had no changes to her treatments or diet since then.
- TSH 3.8 U/mL (optimal range 0.4 – 1.5)
- fT3 1.7 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.8 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin 1400 IU/mL (optimal range <1)
- Anti thyroperoxidase 120 IU/mL) (optimal range <1)
- Ferritin 14 ng/mL (optimal range 70 – 180)
From the things she learned in the program she made a couple of changes:
- Switched to Natural thyroid at a lower dose
- Found out she was anemic and started treating it more effectively
- Stopped taking iodine supplements
- Stopped taking biotin in high doses since it can skew her thyroid tests
- Added back legumes and potatoes to her diet
Anne wrote in to share her excitement about the changes she saw before the end of the 7 weeks:
- “My weight just dropped 10 pounds right after changing my meds!! And I was taking less!!” It has gone down a total of 8 pounds more for a total of 18 pounds.
- Her hair loss also stopped and she’s seeing some early signs of new growth.
Her results also showed major changes:
- TSH 1.8 U/mL (optimal range 0.4 – 1.5)
- fT3 3.7 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.6 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin 235 IU/mL (optimal range <1)
- Anti thyroperoxidase <1 IU/mL) (optimal range <1)
- Ferritin 93 ng/mL (optimal range 70 – 180)
Moving forward Anne is optimistic she will see further weight loss, hair growth, and reduction in her thyroid dosage.
Case study 2
‘Nicole’ signed up for the program mostly because she was not sure if she was on the best thyroid treatment. She was on a new regime as of the last few months and had been getting palpitations, insomnia, and hair loss. She saw a new doctor hoping to lose weight and he put her on a T3 only medication.
She had been doing a low carb diet but had occasional gluten and dairy.
When she started the program she was taking:
- Cytomel 50 mcg
- A multivitamin with folic acid and iodine
- Prilosec OTC for heartburn
- Bone broth protein
Her blood tests were last done just before starting the program. Her prior doctor did not believe in testing her levels but she insisted. He would not test her antibody levels.
- TSH < 0.001 U/mL (optimal range 0.4 – 1.5)
- fT3 8.6 pg/mL (optimal range 2.3 – 4.5)
- fT4 0.7 ng/dL (optimal range 1.09 – 1.9)
From the things she learned in the program she made a couple of changes:
- Found a new physician to work with
- Switched to Natural thyroid at a much lower dose
- Stopped supplements with folic acid due to the cancer risk
- Saw a cardiologist and found her last medication put her in atrial fibrillation
- Changed to a thyroid-specific multivitamin
Over the course of the 7 weeks, Nicole learned that the palpitations, insomnia, and hair loss were all likely side effects of a thyroid dose that was far too high. These symptoms resolved but she’s not yet seen hair regrowth.
Her post program results were much better:
- TSH 0.8 U/mL (optimal range 0.4 – 1.5)
- fT3 3.1 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.3 ng/dL (optimal range 1.09 – 1.9)
- Anti thyroglobulin <1 IU/mL (optimal range <1)
- Anti thyroperoxidase <1 IU/mL) (optimal range <1)
Nicole needed to drop her thyroid dose several times during the 7 weeks. She was surprised when she learned in the program that an overdose of thyroid could cause someone to hold onto extra weight. She did notice her clothes fitting looser as her scores got better.
Her new doctor performed her first ultrasound and saw no signs of Hashimoto’s or other problems with her thyroid. She and her doctor are optimistic and think she may soon not need long-term thyroid treatment.
Case study 3
‘Jackie’ joined the thyroid program because of her severe fatigue and muscle pain. She’d been diagnosed with both fibromyalgia and chronic fatigue over past few years and was on medical disability because the fatigue was so severe. She rated her energy levels between 1-2 out of a possible 10 on most days and 3-4 out of 10 on her best days which happened just a few times per month.
When she started the program she was taking:
- Synthroid 150 mcg
- A multivitamin with folic acid and iodine
- Adderall for focus and energy
- Ambien for sleep
- Soma for muscle pain
Jackie’s last blood tests were last done nearly a year before starting the program. She did not have follow up labs to share.
- TSH 4.1 U/mL (optimal range 0.4 – 1.5)
- fT3 1.6 pg/mL (optimal range 2.3 – 4.5)
- fT4 1.5 ng/dL (optimal range 1.09 – 1.9)
After starting the program she did additional testing and learned some new things.
- She had celiac disease and was not absorbing her medication properly
- She had no thyroid antibodies and a clear ultrasound
- She was positive for chronic Epstein Barr Virus.
Over the course of the 7 weeks of the program, Jackie changed to natural thyroid, did treatment for EBV, and went strictly gluten-free, and started carb-cycling. Jackie was also able to stop her Adderall, Soma, and Ambien.
Some combination of these changes pulled her out of chronic fatigue. First, she was able to regain her natural sleep and get her energy back. She ended the program with energy levels of 6-8 most days.
Recommended episodes